Sleep apnea is a sleep disorder that, if left untreated, can lead to serious health problems such as high blood pressure and heart disease. Untreated sleep apnea causes breathing to repeatedly stop during sleep, resulting in loud snoring and daytime fatigue even after a full nights sleep apnea can affect anyone, but most often it affects older men who are overweight.
Sleep apnea
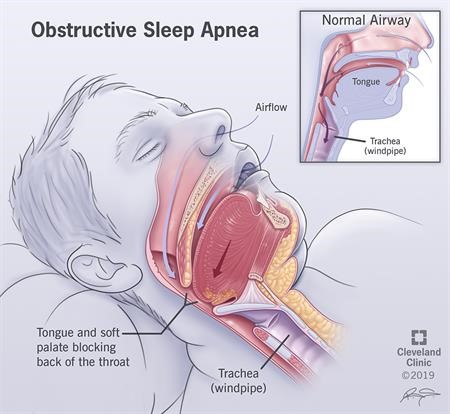
Obstructive sleep apnea occurs when the tongue and soft palate block the airway while you sleep.
What is sleep apnea?
Sleep apnea is a serious sleep disorder that occurs when a person stops breathing during sleep. People with untreated sleep apnea stop breathing repeatedly during their sleep, sometimes hundreds of times throughout the night.
If left untreated, sleep apnea can cause a number of health problems, including hypertension (high blood pressure), stroke, cardiomyopathy (growth of the heart’s muscle tissue), heart failure, diabetes, and heart attack. Untreated sleep apnea can be responsible for school failure, as well as job loss, work-related accidents, and motor vehicle accidents in children and adolescents.
There are two types of sleep apnea, obstructive and central :
- Obstructive sleep apnea is the more common of the two. Obstructive sleep apnea occurs as recurring episodes of complete or partial upper airway obstruction during sleep. During an apnea episode, the diaphragm and chest muscles work harder as pressure increases to open the airway. Breathing usually continues with a loud gasp or body jerk. These episodes can interfere with healthy sleep, reduce oxygen flow to vital organs, and cause heart rhythm irregularities.
- In central sleep apnea , the airway is not blocked, but due to the imbalance in the respiratory control center, the brain cannot signal the muscles to breathe. Central apnea is related to the function of the central nervous system.
Who gets sleep apnea?
Sleep apnea occurs in about 25% of men and 10% of women. Sleep apnea can affect people of all ages, including babies and children, and especially those over 50 and those who are overweight.
Certain physical characteristics and clinical features are common in patients with obstructive sleep apnea. These include excess weight, large neck and structural abnormalities that reduce the diameter of the upper airway, such as nasal congestion, a drooping soft palate, enlarged tonsils, or a small jaw with an overbite.
What Happens When We Stop Breathing During Sleep?
When you stop breathing, your heart rate tends to drop as your body is deprived of oxygen. Then your involuntary reflexes cause you to wake up with a start at the end of the period of not being able to breathe. When this occurs, your heart rate tends to accelerate rapidly and your blood pressure rises.
These are changes that occur acutely when you stop breathing. However, if you experience apnea frequently, your body begins to experience chronic effects. Data shows increased risk, especially when you stop breathing about 30 times per hour or more. However, even at lower frequency rates there is likely to be a risk.
For example, your blood pressure tends to rise, your heart walls thicken due to increased workload, and the structure of your heart changes. Because there are more fibrous cells growing between muscle cells, it tends to be stiffer and less flexible.
All of these increase your risk of having atrial or ventricular arrhythmias. They also tend to reduce the function of the heart so that it is less efficient at pumping blood.
What causes sleep apnea?
Obstructive sleep apnea is caused by a blockage of the airway, usually when the soft tissue at the back of the throat collapses during sleep. Central sleep apnea often occurs in patients with central nervous system dysfunction, such as after a stroke, or in patients with neuromuscular diseases such as amyotrophic lateral sclerosis (ALS, Lou Gehrig’s disease). It is also common in heart failure and other forms of heart, kidney, or lung disease.
What are the symptoms of sleep apnea?
Often the first symptoms of sleep apnea are detected not by the patient, but by his bed partner. Most of those affected have no sleep complaints. The most common signs and symptoms of Sleep Apnea include:
- Snore
- Daytime sleepiness or fatigue.
- Restlessness during sleep, frequent night awakenings.
- Sudden awakenings with a feeling of being out of breath or suffocating.
- Dry mouth or sore throat after waking up.
- Cognitive disorders such as difficulty concentrating, forgetfulness or irritability.
- Mood disorders (depression or anxiety).
- Night sweats.
- Frequent night urination.
- Sexual dysfunction.
- Headache
People with central sleep apnea experience a feeling of suffocation or gasping for air upon awakening and report more frequent repeated awakenings or insomnia.
Symptoms in children may not be as obvious and may include:
- Poor school performance.
- Lethargy or sleepiness is often misinterpreted as laziness in class.
- Daytime mouth breathing and difficulty swallowing.
- The inward movement of the ribcage while breathing.
- Unusual sleeping positions, such as sleeping on hands and knees or with the neck extremely stretched.
- Excessive sweating at night.
- Learning and behavioral disorders (hyperactivity, attention deficit).
- Bedwetting.
DIAGNOSIS AND TESTS
How is sleep apnea diagnosed?
If your doctor determines that you have symptoms suggestive of sleep apnea, he or she may order a sleep evaluation with a sleep specialist or order an overnight sleep study to objectively evaluate sleep apnea.
- The test includes an overnight sleep study called a polysomnogram (PSG). PSG is performed in a sleep laboratory under the direct supervision of a trained technologist. During the test, various body functions are recorded during sleep at night, such as the electrical activity of the brain, eye movements, muscle activity, heart rate, breathing patterns, air flow and blood oxygen levels. After the study is completed, the number of times breathing is disrupted during sleep is calculated and the severity of sleep apnea is rated.
- For adults, a Home Sleep Test can sometimes be done instead. This is a modified sleep study that can be done in the comfort of home. It records fewer body functions than a polysomnogram (PSG), including airflow, respiratory effort, blood oxygen levels, and snoring, to confirm a diagnosis of moderate to severe obstructive sleep apnea.
The Home Sleep Test is not suitable for use as a screening tool in patients without symptoms. It is not used in patients with significant medical problems (such as heart failure, moderate to severe heart disease, neuromuscular disease, or moderate to severe lung disease). It is not for use in patients with other sleep disorders (such as central sleep apnea, restless legs syndrome, insomnia, circadian rhythm disorders, parasomnias, or narcolepsy) in addition to suspected obstructive sleep apnea.
PROCESS AND TREATMENT
What are the treatments for sleep apnea?
Conservative treatments : In mild cases of obstructive sleep apnea, conservative treatment may be all that is needed.
- Overweight people may benefit from losing weight. Even a 10% weight loss can reduce the number of apnea events for most patients. However, it may be difficult to lose weight with untreated obstructive sleep apnea due to the increased appetite and metabolism changes that can occur with obstructive sleep apnea.
- People with obstructive sleep apnea should avoid alcohol and some sleeping pills, which cause further collapse of the airway during sleep and prolong periods of apnea.
- In some patients with mild obstructive sleep apnea, breathing pauses occur only when they lie on their back. In such cases, using a wedge pillow or other devices that help them sleep in a side position may be helpful.
- People with sinus problems or nasal congestion should use nasal sprays or breathing strips to reduce snoring and improve airflow for easier nighttime breathing. Avoiding sleep deprivation is important for all patients with sleep disorders.
Mechanical therapy : Positive Airway Pressure (PAP) therapy is the preferred initial treatment for most people with obstructive sleep apnea. With PAP treatment, patients wear a mask over their nose and/or mouth. An air blower gently moves air through the nose and/or mouth. Air pressure is adjusted to be sufficient to prevent upper respiratory tract tissues from collapsing during sleep. PAP therapy prevents airway closure during use, but apnea episodes return when PAP is stopped or used incorrectly. There are several styles and types of positive airway pressure devices, depending on the specific needs of patients.
Surgery : Surgical procedures can help people with obstructive sleep apnea and others who snore but do not have sleep apnea. Among the many types of surgeries performed are outpatient procedures. Surgery is for people with excessive or malformed tissues that obstruct airflow through the nose or throat, such as nasal curvature, noticeably enlarged tonsils, or a small lower jaw with an overbite that causes the throat to be abnormally narrow. These procedures are typically performed when sleep apnea does not respond to conservative measures and a trial of CPAP. Types of surgery include:
- Somnoplasty is a minimally invasive procedure that uses radiofrequency energy to reduce soft tissue in the upper airway.
- Tonsillectomy is the procedure of removing tonsil tissue in the back of the throat, which is a common cause of congestion in children with sleep apnea.
- Uvulopalatopharyngoplasty (UPPP) is a procedure that increases the width of the airway in the throat opening by removing the soft tissue at the back of the throat and palate.
- Mandibular/maxillary advancement surgery is the surgical correction of certain facial abnormalities or throat blockages that contribute to obstructive sleep apnea. This is an invasive procedure reserved for patients with severe obstructive sleep apnea with head-facial abnormalities.
- Nose surgery involves correcting nasal obstructions, such as a deviated septum.
What are the effects of sleep apnea?
If left untreated, sleep apnea can cause a number of health problems, including hypertension, stroke, arrhythmias, cardiomyopathy (growth of the muscle tissue of the heart), heart failure, diabetes, obesity and heart attacks.
Sleep apnea is likely to cause arrhythmias and heart failure because if you have sleep apnea, you tend to have higher blood pressure. In fact, sleep apnea occurs in approximately 50% of people with heart failure or atrial fibrillation.
This is because sleep apnea can cause:
- Repeated attacks of low oxygen (what doctors call hypoxia).
- Changes in carbon dioxide levels.
- It directly affects the heart due to pressure changes within the chest.
- Increased levels of inflammation markers.
With the high prevalence of sleep apnea in cardiac arrhythmias and heart failure (essentially a coin toss as to whether the patient has it), experts recommend that you do not delay in seeking your doctor’s advice. Please contact me for detailed information.